Obesity and Pregnancy
Obesity, a significant health issue of modern life, not only threatens general health but also has profound and complex effects on reproductive health. For women planning to have children, the relationship between obesity and pregnancy can be a serious obstacle, reducing the chances of conception and introducing various risks. In this article, we will detail the negative effects of obesity on fertility, its connection to Polycystic Ovary Syndrome (PCOS), and the role of bariatric surgery—specifically the positive link between gastric sleeve and pregnancy—in resolving these issues. Our goal is to provide you with information and confidence, illuminating the steps toward a healthy pregnancy.
Obesity is defined as the accumulation of excessive body fat to a degree that impairs health, typically measured by the Body Mass Index (BMI). A BMI over 30 kg/m² is considered obesity. This condition can lead to hormonal imbalances, causing menstrual irregularities, ovulatory disorders, and ultimately, infertility in women. Understanding this complex relationship between obesity and pregnancy is the first step toward the dream of building a healthy family.
How Does Obesity Reduce Fertility?
The negative impact of obesity on the likelihood of pregnancy is not due to a single cause; rather, it is a complex process involving interactions among numerous hormonal and metabolic systems. Excessive fat (adipose) tissue in the body acts like an endocrine organ, disrupting the normal hormonal balance.
Hormonal Imbalances and Ovulation Problems
Adipose tissue produces a type of estrogen called estrone. In obese women, excess fat tissue leads to an overproduction of estrone. This high level of estrogen disrupts the normal function of the hypothalamus and pituitary gland, the brain’s hormone production centers. This disruption causes an imbalance in the secretion of Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH), which regulate ovulation. As a result, ovulation becomes irregular or may stop completely (anovulation). Without regular ovulation, conceiving naturally is not possible.
Insulin Resistance and Its Effects
Obesity often goes hand in hand with insulin resistance, a condition where the body’s cells do not respond adequately to the hormone insulin. To compensate, the pancreas produces more insulin, leading to elevated insulin levels in the bloodstream (hyperinsulinemia). High insulin levels stimulate the ovaries to produce more androgens (male hormones), such as testosterone. Increased androgen levels negatively affect egg development and disrupt the ovulation process. This mechanism forms a strong link with Polycystic Ovary Syndrome (PCOS), which underlies many obesity and pregnancy issues.
The Role of the Leptin Hormone in Reproductive Function
Leptin is a hormone produced by fat cells that regulates the feeling of satiety. Obese individuals have high levels of leptin, but the brain develops a resistance to this hormone (leptin resistance). Elevated leptin levels can interfere with the hormonal signals that regulate reproductive functions, negatively affecting the ovulation process.
The Link Between Obesity and Polycystic Ovary Syndrome (PCOS)
Polycystic Ovary Syndrome is one of the most common hormonal disorders among women of reproductive age and a leading cause of infertility. Symptoms of PCOS include menstrual irregularities, high levels of male hormones in the blood (hyperandrogenism), acne, excessive hair growth, and the formation of multiple small cysts on the ovaries.
There is a strong, bidirectional relationship between obesity and PCOS. Obesity increases the risk of developing PCOS and worsens existing symptoms. Likewise, women with PCOS are more prone to weight gain and obesity. At the center of this vicious cycle is often insulin resistance. As mentioned, obesity-related insulin resistance leads to high insulin levels, which in turn triggers the ovaries to produce excess androgens. These high androgen levels interfere with egg development, disrupt the menstrual cycle, and cause the characteristic symptoms of PCOS. Therefore, obesity acts as both a cause and a consequence of PCOS, and when these two conditions coexist, they have a much more devastating effect on fertility.
The Positive Impact of Weight Loss on Fertility
This strong link between obesity and pregnancy also offers a crucial clue for treatment: weight loss. In obese patients with PCOS, a weight loss of just 5-10% of their body weight can lead to dramatic improvements in hormonal balance.
The mechanisms by which weight loss improves fertility include:
- Increased Insulin Sensitivity: Losing weight increases the body’s sensitivity to insulin. This reduces the pancreas’s need to produce excess insulin, and blood insulin levels fall.
- Lower Androgen Levels: Decreased insulin levels suppress the ovaries’ overproduction of androgens. The reduction of male hormones in the bloodstream allows for normal egg development.
- Regulation of the Menstrual Cycle: With the restoration of hormonal balance, a large percentage of women experience the return of regular menstrual cycles and spontaneous ovulation.
- Increased Chance of Natural Conception: The return of regular ovulation significantly increases the probability of conceiving naturally. This is particularly hopeful for women planning for sleeve gastrectomy and pregnancy.
In short, addressing obesity corrects the underlying metabolic disorders of PCOS, alleviating the syndrome’s symptoms and restoring fertility. For obese women with PCOS who wish to have children, the first and most important treatment step is to achieve healthy and sustainable weight loss.
The Most Effective Treatment for Obesity: Bariatric Surgery
Diet, exercise, and lifestyle changes are the cornerstones of weight loss. However, for individuals with morbid obesity (BMI > 40 kg/m² or BMI > 35 kg/m² with associated health conditions), the weight loss achieved through these methods is often insufficient and temporary. For this patient group, the most scientifically proven and lasting weight loss method is bariatric surgery.
What is Sleeve Gastrectomy?
Sleeve gastrectomy, also known as stomach reduction surgery, involves the laparoscopic (closed) removal of about 80% of the stomach. This procedure reshapes the stomach into a thin tube or banana shape. The primary goal of the surgery is twofold: to restrict the amount of food a patient can consume in one meal and to reduce appetite by removing the part of the stomach that secretes the hunger hormone, Ghrelin. This dual effect helps patients feel full with less food and experience prolonged satiety, leading to effective and permanent weight loss.
The Effects of Bariatric Surgery on Fertility
Bariatric surgery not only provides effective weight loss but also significantly corrects the hormonal and metabolic disorders caused by obesity. The positive relationship between gastric sleeve and pregnancy is helping many women realize their dream of motherhood.
- Rapid and Lasting Weight Loss: Patients typically lose 60-80% of their excess weight within the first 1-2 years after surgery. This significant weight loss is the foundation for the positive effects on fertility.
- Resolution of Metabolic Syndrome: Bariatric surgery rapidly corrects insulin resistance. In some patients, blood sugar and insulin levels return to normal just days after surgery, even before significant weight loss occurs. This is a revolutionary development in the treatment of PCOS.
- Hormonal Balance and Return of Ovulation: With the normalization of insulin and androgen levels, the vast majority of patients experience regulated menstrual cycles and the return of spontaneous ovulation. Studies show that over 70% of women with PCOS who undergo bariatric surgery have their periods regulate and their infertility issues resolve.
- Increased Chance of a Healthy Pregnancy: The elimination of obesity not only increases the chance of conception but also ensures a healthier pregnancy. Risks associated with obesity and pregnancy, such as gestational diabetes, high blood pressure (preeclampsia), large-for-gestational-age babies, preterm birth, and the need for a cesarean section, are significantly reduced.
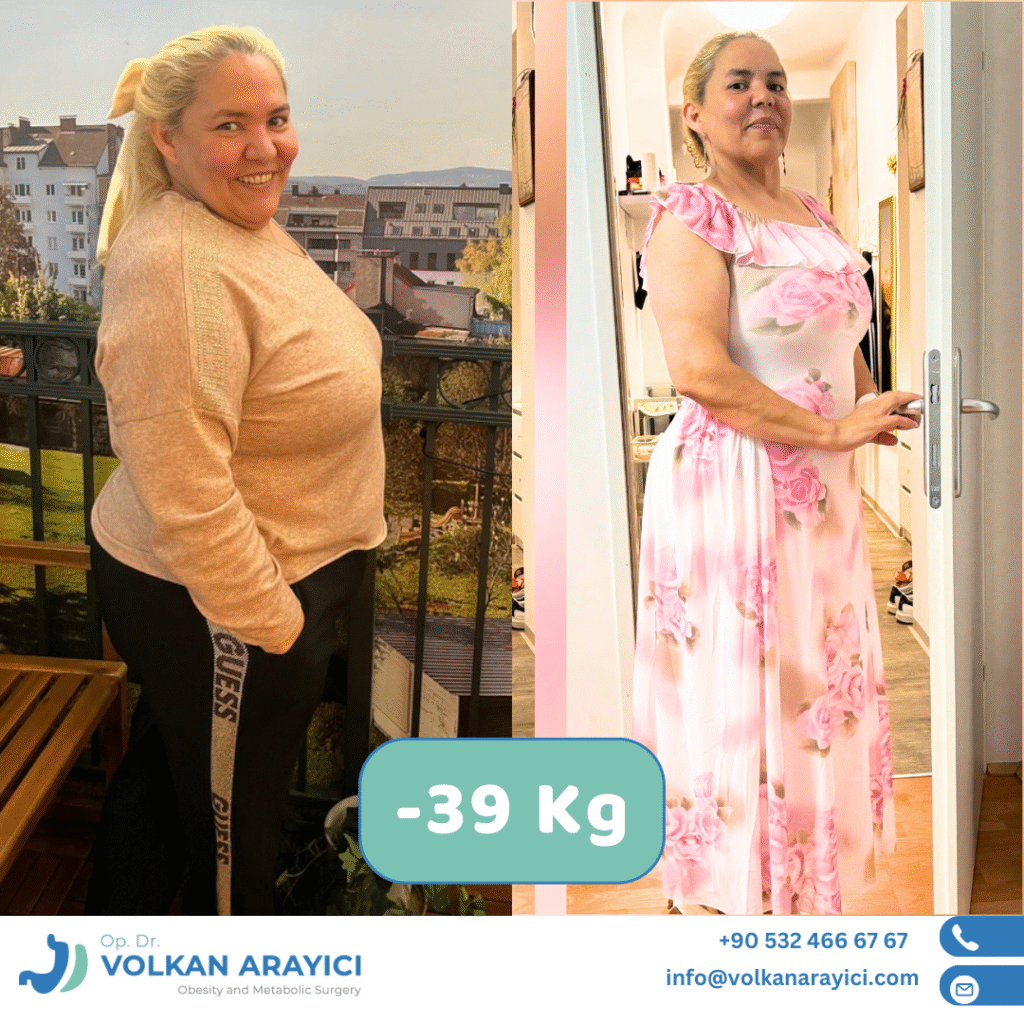
Success Stories of Reaching Dreams with Op.Dr. Volkan Arayıcı
The best way to illustrate the positive relationship between gastric sleeve and pregnancy is through our patients’ own success stories. Here are the stories of three of our patients who trusted Op.Dr. Volkan Arayıcı and achieved their dreams:
- Ayşe’s Miracle: After years of struggling with PCOS and a weight of 120 kg, Ayşe was about to lose hope after numerous failed treatments. After meeting Op.Dr. Volkan Arayıcı, she decided to have a sleeve gastrectomy. A year after the surgery, she lost 45 kg, approaching her ideal weight. Her menstrual cycle became regular, and shortly thereafter, she received the joyful news that she was pregnant naturally.
- Fatma’s New Beginning: Fatma’s general health had deteriorated due to insulin resistance and obesity, and she was unable to get pregnant. Her life completely changed after a successful sleeve gastrectomy performed by Op.Dr. Volkan Arayıcı. As she lost weight, her insulin resistance disappeared, and 18 months after the surgery, she gave birth to a healthy baby.
- Zeynep’s Hopeful Journey: Joint pain and hormonal disorders caused by obesity had diminished Zeynep’s quality of life. Her desire to become a mother seemed impossible due to these problems. Zeynep decided to undergo sleeve gastrectomy. After the surgery, she regained her health and lost her excess weight. Once her body found its balance, she conceived the baby she had so longed for.
Planning for Pregnancy After Bariatric Surgery
For women planning pregnancy after bariatric surgery, timing is the most critical point. Due to rapid weight loss and metabolic changes in the body, pregnancy is not recommended for the first 12-18 months after surgery. This period is a stabilization phase where the body adapts to its new weight and nutrient stores are balanced. After this period, pregnancy can be safely planned under a doctor’s supervision. Regular intake of vitamin and mineral supplements during this time is crucial for the health of both the mother and the baby.

Step into a New Life
Obesity may seem like an insurmountable obstacle to your dream of having a child. However, it is important to remember that this is not your destiny. Modern medicine, especially advances in bariatric surgery, offers you the opportunity to permanently solve this problem and step into a healthier future. By overcoming obesity, you not only regain your fertility but also improve your overall quality of life by resolving many related health issues like diabetes and hypertension.
If you are also struggling with issues related to obesity and pregnancy, do not hesitate to consult a specialist. An experienced bariatric surgery team can create the most suitable treatment plan for you and guide you on your journey to becoming a healthy mother. Remember, a healthy start is the most valuable step you can take for your future and the future of your baby.
Frequently Asked Questions About Obesity and Pregnancy
What is the link between obesity and pregnancy? Does obesity make it harder to get pregnant?
Yes, obesity can negatively affect fertility. Excess body fat can lead to hormonal imbalances, disrupting the regularity of ovulation. It can trigger or worsen conditions like Polycystic Ovary Syndrome (PCOS), causing menstrual irregularities and infertility. Therefore, weight management is crucial for women planning for obesity and pregnancy.
Will losing weight increase my chances of getting pregnant?
Absolutely. In women with obesity, even a weight loss of 5-10% of body weight can significantly improve hormonal balance. Losing weight reduces insulin resistance, lowers androgen (male hormone) levels, and helps regulate the menstrual cycle. This promotes regular ovulation, increasing the likelihood of conceiving naturally.
What is the relationship between gastric sleeve and pregnancy? Can I get pregnant after the surgery?
Yes, sleeve gastrectomy has a very positive effect on fertility. The surgery provides effective and lasting weight loss, correcting the hormonal disorders associated with obesity. As insulin resistance is resolved and hormones balance, many women experience the return of regular ovulation. This is the most significant positive link between gastric sleeve and pregnancy, helping many women achieve their dream of motherhood.
How long after sleeve gastrectomy is it safe to get pregnant?
Generally, pregnancy is not recommended for the first 12-18 months following bariatric surgery. This period is a critical stabilization phase where the body adapts to rapid weight loss and nutrient stores are balanced. After this period, you can safely plan a pregnancy with your doctor’s approval and monitoring.
What are the risks during an obesity and pregnancy journey?
When obesity and pregnancy coexist, certain risks increase for both the mother and the baby. These risks include gestational diabetes, high blood pressure (preeclampsia), having a large baby (macrosomia), preterm birth, and an increased need for a cesarean section. Losing weight significantly reduces these risks.
Do Polycystic Ovary Syndrome PCOS and obesity cause infertility?
Yes, PCOS and obesity are among the most common causes of infertility. Obesity exacerbates PCOS symptoms, and PCOS makes weight gain easier. This vicious cycle, driven by insulin resistance and hormonal imbalances, hinders ovulation and makes it difficult to conceive.
How does sleeve gastrectomy help women with PCOS get pregnant?
Sleeve gastrectomy effectively resolves insulin resistance, the underlying metabolic problem in PCOS. With weight loss and the normalization of insulin levels, the ovaries’ excess androgen production is suppressed. This helps regulate the menstrual cycle and restore spontaneous ovulation, greatly increasing the chances for women with PCOS to conceive naturally.
What should be considered during a pregnancy after sleeve gastrectomy?
In a pregnancy after surgery, close medical follow-up is essential for the health of both the mother and the baby. It is particularly important to take vitamin and mineral supplements (iron, calcium, B12, folic acid) regularly. This process should be managed by a team consisting of a bariatric surgeon, an obstetrician, and a dietitian.
Can I get pregnant just by losing weight through diet and exercise?
Diet and exercise are the foundation of weight loss and may be sufficient to restore fertility in some women. However, for individuals with morbid obesity (BMI > 40), achieving sustainable and adequate weight loss with these methods is often difficult. At this point, bariatric surgery comes into play as a more effective and lasting solution for those considering gastric sleeve and pregnancy.
Who should I consult for obesity treatment?
If you are experiencing issues related to obesity and pregnancy, it is recommended to first consult a bariatric and metabolic surgery specialist. An expert physician will evaluate your condition, determine the most suitable treatment method for you—such as diet, exercise, or surgery—and guide you on the path to a healthy pregnancy.
